The price to remove a gall bladder or replace a hip has spiked more than 20 percent during the past five years, according to an analysis of data collected for NBC News.
Surgery has bloomed into a $500 billion industry in the United States, where 80 to 100 million procedures are performed annually — a per-capita rate that’s some 50 percent higher than in the European Union, said Dr. John Birkmeyer, a researcher and adjunct professor at the Dartmouth Institute and in the university's Community & Family Medicine program.
The reason? Expensive yet safer technologies and hospital consolidations that create medical monopolies, according to doctors and researchers.
For hospitals, surgery is the No. 1 revenue source. That encourages medical center administrators to ensure operating suites remain humming — an assembly-line mentality that can lead to unnecessary procedures and spiraling prices, experts say.
“The cost of surgery is growing at a surprising rate,” said Birkmeyer, a leading researcher on healthcare trends. He bases his calculations on national Medicare claims data.
A price check on four of the most common procedures reveals the inflationary trends hitting ORs since 2009:
- Hernia repair, up 16 percent, with a "total fair price" of $5,056, according to Healthcare Bluebook.
- Gall bladder removal, up 21 percent, with a "total fair price" of $5,532.
- Hysterectomy, up 19 percent, with a "total fair price" of $11,780.
- Hip replacement, up 24 percent, with a "total fair price" of $22,606.
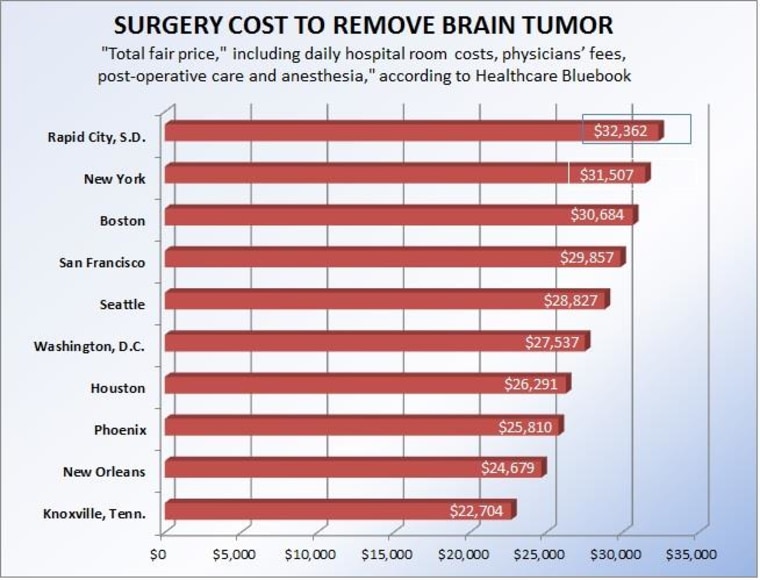
The cost-increase data was generated for NBC News by Healthcare Bluebook, an online guide that helps consumers shop for the best prices in their areas for various medical services. The dollar amounts show the “total fair price” for each surgery as estimated by the website.
Overall, health care inflation has averaged about 4 percent per year during the past five years, Dr. Jeffrey J. Rice, chief executive officer of Healthcare Bluebook, based in Brentwood, Tennessee.
Further causing surgical costs to surge: The U.S. health care economy is built on a tilted foundation. Insurance-company contracts can vastly differ from one hospital to another just blocks away, skewing prices for the same treatments.
“There is almost always a 500 percent — or more — variation for health care services in most cities,” Rice said. “For example, an MRI may cost $500 at one facility and over $3,000 at another facility across the street.”

Surgeons know this, of course. Their fees, dictated by insurance contracts or by Medicare, are included in the overall price of any operation.
“I can take out a gall bladder, and a surgeon in the next room can take out another gall bladder, but he or she may be with a different network of doctors or a different hospital system that negotiated better (insurance) contracts,” said Dr. Paul A. Ruggieri, a general surgeon in Fall River, Massachusetts. “He or she can get paid 20 to 30 percent more than what I get paid regardless of the outcome.”
Those hospital “systems” and doctor “networks” are rooted in a consolidation of care that’s been steadily gobbling up a greater share of the U.S. medical landscape and are a chief driver of the rising surgical prices, according to Birkmeyer, Rice and Ruggieri.
“Hospitals and their pricing systems have, for a very long time, been shielded from competitive market forces,” said Ruggieri, author of “The Cost of Cutting,” out Tuesday. “Hospitals have been allowed to charge whatever they want to charge to third-party payers (insurers). There’s been no transparency to the public in how hospital pricing is determined.”
And as more local hospitals end competitions and merge, the idea of winning new patients through lower prices vanishes, the experts said.
"There’s been no transparency to the public in how hospital pricing is determined."
Consider Boston. In 1994, Massachusetts lawmakers allowed Brigham and Women’s Hospital and Massachusetts General Hospital to consolidate into a one system known as Partners HealthCare. According to the New York Times: “Investigations by the state attorney general’s office have documented that the merger gave the hospitals enormous market leverage to drive up health care costs in the Boston area by demanding high reimbursements from insurers that were unrelated to the quality or complexity of care delivered.”
The Affordable Health Care Act — or Obamacare — fueled even more hospital consolidations, Birkmeyer asserts.
The law created Accountable Care Organizations (ACOs) that “incentivize doctors and other providers to work together to provide more coordinated care to their patients,” former Health and Human Services Secretary Kathleen Sebelius wrote in March 2013. These ACOs “agree to take responsibility for the cost and quality of their patients’ care, (and) to improve care coordination and safety.”
They also boost the costs of surgeries, Birkmeyer asserts.
“That drive toward hospitals forming bigger conglomerations of networks and physician practices has reduced competition, and in a non-Medicare population, has enabled hospital systems in many parts of the country to charge far more,” Birkmeyer said.
At the same time, OR innovation — great for patients, tough on wallets — has bumped up surgery prices.
Those tech advances include robotic surgeries, now performed hundreds of thousands of times a year for certain procedures, including hysterectomies. A doctor sits near the operating table at a console, where he or she can manipulate robotic arms while watching through a 3-D viewfinder.
“Those have very positive effects in respect to recovery or the risks of complications for patients,” Birkmeyer said.
“But technology is very costly for hospitals and, ultimately, those costs get passed to insurers — and to the rest of us.”