The World Health Organization says it has set up an emergency committee of experts to keep an eye on the new MERS virus that’s killed 42 people, most of them in Saudi Arabia.
There’s no evidence the virus has started to cause a pandemic – a global outbreak of disease. And a study published on Friday shows that by one measure, the virus isn’t infectious enough to cause one – yet.
But WHO and other health experts say the virus is very worrying.
"We want to make sure we can move as quickly as possible if we need to,” said Dr. Keiji Fukuda, WHO’s top flu expert.
"If in the future we do see some kind of explosion or if there is some big outbreak or we think the situation has really changed, we will already have a group of emergency committee experts who are already up to speed so we don't have to go through a steep learning curve,” Fukuda told a news conference.
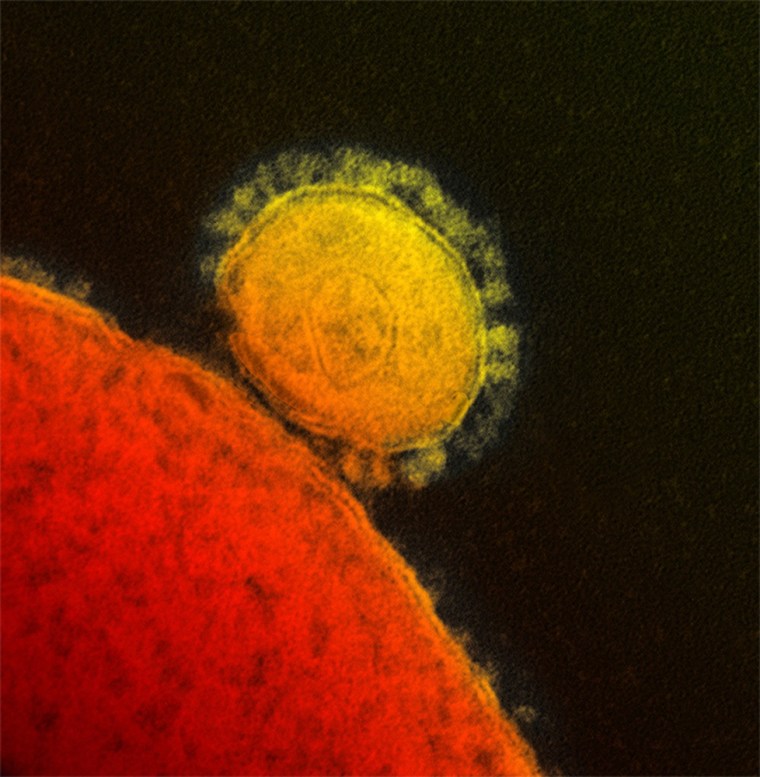
MERS (short for Middle East respiratory syndrome) broke out just over a year ago in Saudi Arabia. WHO has official confirmation of 79 cases and 42 deaths – a rate that shows the virus is extremely deadly.
One of the latest deaths – a Qatari man who had been in a London hospital since September.
A single patient can infect many others. MERS is a relative of the severe acute respiratory syndrome (SARS) virus that spread globally from China in 2003, killed 775 people and infected close to 800 before it was stopped.
SARS spread in what are known as clusters in which certain people seemed to be far more infectious than others. These “superspreaders” infected groups of health care workers or others they came into contact with. There’s some evidence MERS might spread that way sometimes, too, although not always.
And any virus is just an airplane ride away from anywhere else in the world. SARS spread slowly within China for weeks or months before travelers carried it globally. In one notorious instance, an infected traveler became sick and threw up in a Hong Kong hotel. He infected seven other people, who eventually carried the virus to Canada, Vietnam, Singapore and elsewhere in Hong Kong.
MERS has been reported in Jordan, Qatar, Saudi Arabia, and the United Arab Emirates (UAE), France, Germany, Italy, Tunisia and Britain. MERS has not been seen in the United States, although a handful of travelers have been tested for the virus, according to the Centers for Disease Control and Prevention.
One reason experts are especially worried about MERS is that it has spread in hospitals and clinics. Also, Saudi Arabia will host the annual Hajj, with its influx of millions of observant Muslims from all over the world, in October.
But there’s some reassuring news. A French team has calculated the infectiousness of MERS and found it’s not yet as transmissible as measles, smallpox or even flu in a bad year.
Arnaud Fontanet of the Pasteur Institute in Paris and colleagues looked at a measure called R0, which reflects how many other people an infected person might transmit a disease to.
“When R0 is above 1, epidemic potential has been reached,” Fontanet’s team writes in the Lancet medical journal.
“With our most pessimistic scenario, we estimated MERS-CoV (MERS coronavirus) R0 to be 0.69; by contrast, the R0 for prepandemic SARS-CoV (SARS coronavirus) was 0.8,” they added.
“Our analysis suggests that MERS-CoV does not yet have pandemic potential.”
To compare, R0 for measles and whooping cough is 12 or higher in unvaccinated groups, for polio it’s between 5 and 7, and for HIV it’s between 2 and 5.
Researchers found after SARS was over that it had repeatedly passed from animals to people in China, mutating in the process until it took on a form that more easily infected people and that more easily passed from person to person.
“The same sequence of events might be occurring with MERS-CoV, which has been repeatedly introduced into the human population for more than a year (from an unknown animal host) and might have human pandemic potential,” Fontanet’s team wrote.
SARS was eventually traced to bats and an animal called a civet, a delicacy in China. Scientists suspect MERS also comes from an animal, but they haven’t been able to find the source yet.