As hospitals around the country prepare for an increased number of coronavirus patients and potential bed shortages, local officials seek hotel rooms and dorms as alternative housing for coronavirus patients with less severe symptoms.
In Los Angeles County, the Fairplex Sheraton Hotel has been designated a medical shelter and had 25 COVID-19 patients Friday.
San Francisco has secured leases for over 300 hotel rooms. It plans to finalize the leases of 3,000 more this week.
In New York, local officials and the U.S. Army Corps of Engineers are touring hotels and State University of New York residence halls.
But how do you turn a hotel room into a health care room?
The first step is understanding that the coronavirus is primarily spread by respiratory droplets.
Full coverage of the coronavirus outbreak
Dr. Peter Chin-Hong, an infectious disease specialist at the University of California, San Francisco, likened its transmission to a droplet of water, which is heavy and falls onto a surface. By comparison, airborne diseases like measles are more like dandelion seeds, which are light and can linger in the air. The latter require much more complex measures.
The next step is determining what kind of patients are going to be housed. A person who tested positive but needs only to be isolated to reduce spread has different needs from someone who's intubated and on a ventilator.
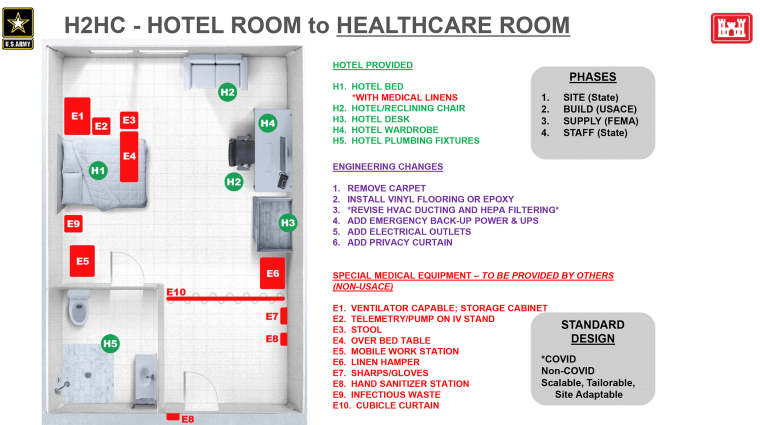
The Army Corps of Engineers issued guidance, called the "Hotel to Healthcare Concept," that local and state governments can rely on to prepare rooms for a range of patients. (The Army Corps' concepts are implemented by contractors and paid for by money from the Federal Emergency Management Agency.)
To handle patients with more serious COVID-19 symptoms, the Army Corps recommends adding the following to rooms: a bedside table or a cabinet that can hold a ventilator, an over-bed table or tray for patients, a mobile work station for medical personnel, an IV stand, a linen hamper for soiled items, a puncture-proof box for needles and gloves, a receptacle for infectious waste and a hand sanitizer station.
It also recommends several more labor-intensive changes, including adding privacy curtains near the front door, removing carpet to cut down on contamination, installing vinyl flooring and adding electrical outlets and emergency backup power.
COVID-19 isn't typically spread through airborne transmission, but certain procedures, such as intubation, can make the respiratory droplets more aerosolized. For patients who need this level of care, hotel rooms and dorms with their own air conditioning units can be converted into negative pressure rooms.
Lt. Gen. Todd Semonite, commanding general of the Army Corps of Engineers, said in news briefings that the "relatively simple" conversion process involves adjusting the air conditioning to suck more air out of the room through the vents. A big piece of plastic with a zippered entry would be placed over the door, and the resulting negative pressure would prevent contaminated air from escaping the room.
The Army Corps' "Hotel to Healthcare Concept" also includes suggestions beyond those for individual rooms.
Nurse stations should be set up near the elevators on each floor, and generators should be brought in. Patient screening tents and exterior pharmacies should be set up, and medical waste disposal areas should be designated.
The concept is meant to inform local public officials, but it's obviously not feasible to implement every change in hotel rooms or dorms before they're needed. Many are also unnecessary if the site is admitting only patients with less severe symptoms.
But regardless of the type of patient, every hotel or residence hall should have security, medical personnel and food and laundry services onsite to care for patients.
Those are four measures the Fairplex Sheraton implemented immediately, according to Helen Chavez, assistant director of the Los Angeles County Office of Emergency Management.
The hotel didn't undergo an extensive makeover, but so far it has been tasked only with admitting COVID-19 patients who aren't in critical condition and people with symptoms who are awaiting test results.
Chin-Hong said that even for less serious COVID-19 patients, rooms still need a minimum number of key things.
Personal protective equipment, such as masks, gloves, gowns and hand sanitizer, as well as inexpensive bins to dispose of infectious waste, should be in each room. Few personal items should be allowed besides a phone or a computer that connect patients to the outside world and can easily be disinfected. Signs with basic reminders and protection steps should be posted around the building.
Download the NBC News app for full coverage and alerts about the coronavirus outbreak
Rooms should be as bare as possible. (More comfort for hotel guests and students means more surfaces for contamination.) Because it's not always possible to remove excess furniture, deep cleaning is crucial before and after each new patient.
Cleaners would focus on disinfecting high-touch surface areas, such as doorknobs, handles and light switches. Because it's not an operating suite, there's no need to clean the ceilings or the walls, said Pratik Shinde, who owns a ServiceMaster franchise that offers health care sanitizing.
He said properly decontaminating a standard hotel room takes about 30 minutes. The average hotel room is 325 square feet, and the average dorm room is less than half that.
It's important to note that medical, government and hospitality experts who spoke with NBC News agreed that the most critical cases ideally should be housed in hospitals. But for those with less severe symptoms, alternative housing is a viable solution that could cut down on hospital numbers and help isolate the infected.
As the coronavirus continues to affect more of the country, the Army Corps of Engineers has been working closely with more local authorities to quickly prepare for the worst.
