A test for HPV, the virus that causes cervical cancer, works just as well as a Pap smear for finding pre-cancerous changes in women, researchers reported Tuesday.
In fact, it might even work better at detecting the pre-cancerous changes that lead to cervical cancer, the Canadian team found.
The study, published in the Journal of the American Medical Association, adds to a growing body of evidence that HPV tests may be superior to Pap smears. Eventually, women may be advised to get only an HPV test.
The human papillomavirus (HPV) causes 99 percent of all cases of cervical cancer, according to the National Cancer Institute.
It also causes head and neck cancer, anal cancer and cancer of the penis. Cervical cancer still affects more than 12,000 women in the U.S. every year and kills more than 4,000.
There’s a vaccine that prevents most cancer-causing strains of HPV, but once a person has become sexually active, it’s too late to get it. The vaccine is given to teens and young adults, but generations of women are still at risk of cervical cancer because HPV eventually infects most people at some point.
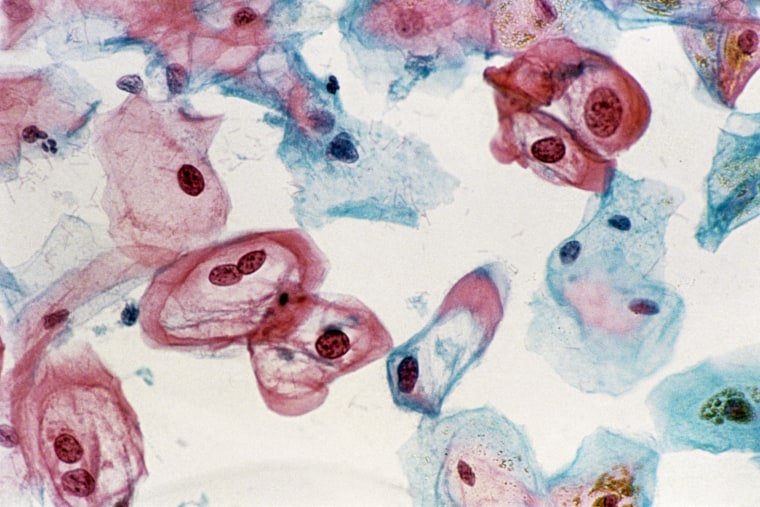
The Pap test is a smear taken regularly to look for the changes that indicate cancer is developing on the cervix. If the changes are there, doctors can remove the damaged tissue and prevent cancer from ever developing.
It’s now clear that HPV is the cause of those changes almost all the time, and detecting HPV is a good way to screen women for cervical cancer.
Which test is better?
Dr. Gina Suzanne Ogilvie of the Women’s Hospital and Health Center in Vancouver and colleagues set up a comparison study. They recruited 19,000 women to agree to get either an HPV tests or a standard Pap test. After four years, all the women also got tested with both types of test.
This kind of randomized clinical trial is considered the best way to tell if one treatment or test works better than another.
After four years, the women who got HPV tests were less likely to have serious changes that can lead to cervical cancer, a diagnosis of cervical intraepithelial neoplasia 2 or 3 (CIN2 and CIN3), Ogilvie’s team found.
“These results have demonstrated that primary HPV testing detects cervical neoplasia earlier and more accurately than cytology,” they wrote.
The older test missed the early pre-cancerous changes in more than 300 women, the team said.
“These results are exciting as they will help us move towards simpler and more effective screening, which along with the preventive HPV vaccine will help significantly decrease cervical cancer deaths for women all over the world,” said Dr. Kathleen Schmeler, an expert in women’s cancers at The University of Texas MD Anderson Cancer Center.
“This information will help inform future cervical cancer screening guidelines and continue to decrease deaths from this preventable disease,” added Schmeler, who was not involved in the study.
Both tests are given in the same way, via a smear, so a woman’s experience in the doctor’s office would not be different if she had an HPV or older Pap test.
But there have been some barriers to just replacing the older test with an HPV test, said Dr. Stewart Massad of Washington University School of Medicine in St Louis.
That’s because HPV is a very common infection, but usually people clear it very quickly on their own with no symptoms. It only lingers or comes back in some people, for reasons that doctors cannot yet predict.
So the HPV test comes back positive for many younger women who are newly infected but who will probably clear it without it causing the damage that leads to cancer.
Also, women don’t understand that a positive HPV test doesn’t mean they just got infected, Massad said in a commentary in the same journal.
“HPV may recur and first be detected decades later in the context of long-term monogamy or abstinence,” wrote Massad, who helped advise the Food and Drug Administration on approving the first HPV cervical cancer screening test.
“Communicating a positive HPV test result requires sensitivity by the clinician,” he added. “Women will need to understand the importance of testing for these sexually transmitted viruses, including that HPV infections are almost ubiquitous, may regress, and can be followed without therapy unless progressing toward cancer.”
Groups such as the American Cancer Society now recommend that women over 30 get tested with both HPV and standard cell-based Pap tests every five years. The U.S. Preventive Services Task Force, which makes recommendations for doctors, recommends Pap tests every three years for women over 21 or a combination of both Pap and HPV tests every five years for women over 30.
It is considering a change, recommending HPV testing alone every five years for women over 30.

