Tammy Mathews was working a late-night Sunday shift in an Alabama emergency department when a patient, drunk and high on drugs, grabbed her around the neck, choked her until she couldn’t breathe -- and then spat in her face.
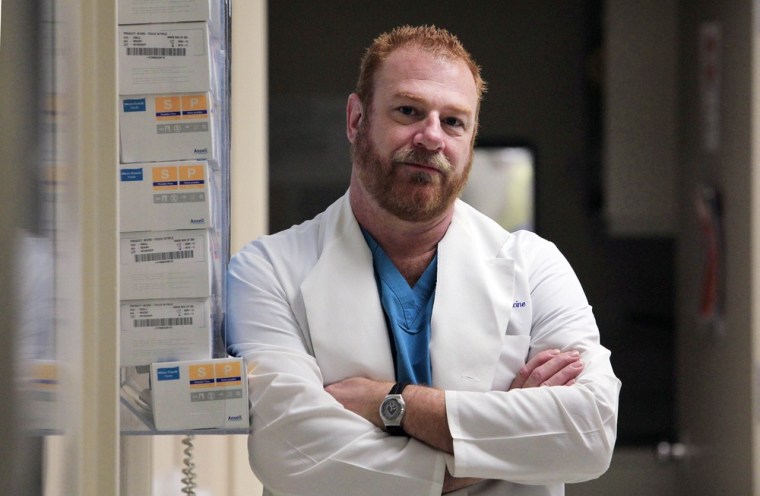
Jeaux Rinehart was staffing a Seattle emergency room when a patient in a triage room, upset that he couldn’t get methadone, pulled a billy club out of a backpack and beat Rinehart in the back of the head and across the face, breaking his cheekbone.
So neither Mathews nor Rinehart was surprised to learn that an ongoing poll of nearly 7,200 emergency nurses finds that violence in the ER remains high, despite increased attention to a problem that leaves some health workers worried about danger every day.
“It’s so global,” said Rinehart, 51, president of the Washington State Emergency Nurses Association. “It’s actually getting worse.”
According to latest figures from the national Emergency Nurses Association, between January 2010 and January 2011, more than half of nurses in the ER -- 53.4 percent -- reported experiencing verbal abuse and about 13 percent said they had encountered physical violence at work in the previous week.
Being grabbed or pulled was the most common physical assault, while yelling and swearing were the most common kinds of verbal attack.
That’s about the same rate previously detected by the ongoing survey conducted by the ENA starting in May 2009. The Des Plaines, Ill., association surveys nurses at three-month intervals, partly to determine if the problem is getting any better, said AnnMarie Papa, the group’s president.
Frustrated, she admitted that it isn't.
“It’s upsetting to me that we can’t change the culture,” Papa said. “What is this with society that says it’s OK to do this to people who are trying to help them?”
Nurses on the front lines, like Mathews, 49, of Auburn, Ala., say that long waits, crowded conditions and growing numbers of mentally disturbed patients all exacerbate the stress of emergency department visits.
“Tempers kind of flare up and it just happens,” said Mathews, who was assaulted in 2005.
Both Mathews and Rinehart have worked in emergency departments for decades and they say they’ve come to expect vile treatment by patients and their families.
“I’ve been called things that, honestly, I have never even thought about putting those words together,” said Rinehart, who was attacked with the club in 2007.
The problem has received serious attention in recent years. At least 25 states have strengthened penalties for attacking health care workers and a growing number of hospitals have bolstered both physical security measures and staff training, according to the American Hospital Association.
At Virginia Mason Medical Center in Seattle, the hospital where Rinehart works, a new emergency department opened just last week with greatly enhanced security features, among other amenities, according to spokesman John Gillespie.
But that progress hasn’t curbed the crisis, said Papa, who advocates a zero-tolerance policy to stop ER violence. Only about a third of nurses actually submit formal reports about physical violence and less than 15 percent report verbal assaults, the survey found. That might be because in almost half of cases of physical violence -- 46.7 percent -- no action was taken against the perpetrators. In nearly three-quarters of cases -- 71.8 percent -- nurses received no response from hospital officials about the assaults.
In Mathews’ case, she said the hospital wanted her to drop assault charges against her attacker, and that officials fired her when she refused. She works in the emergency department of a different hospital now and she says she's still wary of erratic patients. Rinehart said he has transferred out of the emergency department to focus instead on patient safety.
“I miss it, but I don’t miss being called every name in the book," said Rinehart, who worked in ERs for 32 years. "I miss it, but I’m not going back.”