Cancer patients are all too familiar with the debilitating effects of chemotherapy, still a mainstay of treatment for many malignancies. But as some researchers work to find new drugs, others are working to create new drug-delivery tools. Some of that work involves hacking things like virus particles and bee venom— even sperm cells.
The goal of the research is to find ways to target the delivery of cancer drugs more effectively in order to boost their effectiveness and alleviate side effects— which in some cases are no less dangerous than the cancer itself.
“Some chemotherapy drugs can destroy patients’ hearts or kidneys,” says Daniel Kohane, a Harvard Medical School professor whose lab conducts research on biomaterials and drug delivery.
Chemotherapy works essentially by killing fast-growing cells. But cancer cells aren’t the only ones in the body that reproduce rapidly. Cells in the intestinal lining turn over quickly. Ditto for hair follicles and blood cells. So as chemo takes on cancer cells, it’s also damaging healthy cells.
“Only about 0.1 percent of the drug molecules actually reach and go into the tumors,” says Haifa Shen, an associate professor of nanomedicine at the Houston Methodist Research Institute who studies drug delivery methods. “Over 99.9 percent of chemo drug molecules stay outside of the tumors, being very toxic to normal tissues.”
VIRUSES VS. BREAST CANCER
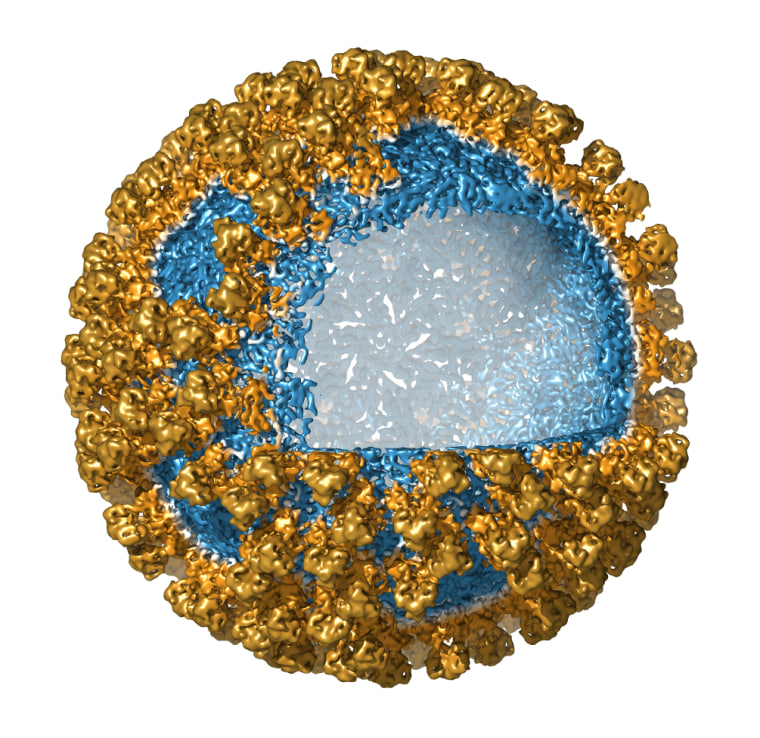
Viruses are promising drug-delivery tools because, once inside the body, they’re great at finding their way to specific types of cells while avoiding other types. Cold viruses target cells lining the nose, throat, and lungs, for example, while the Ebola virus attacks cells in the liver and arteries. Once inside their target cells, viruses unload their cargo of genetic material and set the stage for the production of more virus particles.
It would be a major advance in cancer therapy if researchers could find a way to modify viruses so as to retain their targeting capabilities while swapping out their genetic cargo for potent anticancer molecules. And Frank Sainsbury and his team at the University of Queensland in Australia are doing just that. In a series of preliminary experiments, the scientists created “fake” viruses whose outer shells, or capsids, were engineered to attach only to breast cancer cells.
“It’s somewhat similar to how two magnets interact with each other, and we can build the capsid’s surface that way,” Sainsbury says.
Sainsbury started off with Bluetongue, a virus that affects only cows and sheep. Using tobacco plants as incubators, the team created empty Bluetongue capsids and then loosed them on breast cancer cells in a petri dish. The shells did what the scientists hoped they would. They found their targets, and the cancer cells “took them in,” according to Sainsbury.
Bluetongue shells make good drug delivery vehicles because they can carry a lot. “They are big shells with a lot of cargo space that we can fill with drug molecules,” Sainsbury says. He added that the next step for his research will be to load the shells with chemo drugs and get them to unload their cargo to kill tumors.
MODIFIED BEE VENOM
Cancers vary in lethality, and brain cancer is often a death sentence— in part because few drugs are able to reach the brain.
The brain is separated from the rest of the body by a protective membrane that keeps out microbes, viruses, and other potentially harmful organisms and substances. “Your brain is like a medieval city surrounded by stonewalls with the guards at the gates that select who can go through,” says Ernest Giralt, a professor of organic chemistry at the University of Barcelona in Spain. “So very few chemicals can get into the brain.”

Luckily, some substances are able to sneak in. One is bee venom, or apamin, which bees release when they sting.
In its original form, apamin can’t be used therapeutically because it harms nerve cells. So Giralt’s team chemically modified apamin to take away the molecule’s toxic effects. The team injected mice with the modified apamin and observed no side effects. And the modified apamin crossed the brain membrane even more easily than the original version. “It was pure serendipity," Giralt says.
The team is now exploring the best way to use apamin to shuttle chemo drugs into the brain. There seem to be two ways to do it, Giralt says. One would be simply to attach a chemo molecule to modified apamin. The other would be to fashion a sort of “bulk shipment”— basically stashing a load of chemo into a virus shell studded with apamin molecules and testing whether it can pass through the membrane.
‘SPERMBOTS’ TO THE RESCUE
Hardly anyone would think of sperm as a tool to fight cancer, but a group of researchers at IFW Dresden and Chemnitz University of Technology in Germany did. Their preliminary research suggests that it might be possible to turn sperm into “sperm-hybrid micromotors” able to deliver chemotherapy agents to malignancies of the cervix, ovaries, or uterus.
Sperm, of course, have evolved to navigate the female reproductive tract. They neither damage tissue nor cause toxic side effects. To create the spermbots, the scientists soaked bull sperm cells in the cancer drug doxorubicin and then “dressed” the cells with tiny iron-coated mesh. Then they used magnets to steer the cells toward tumor cells in a petri dish.
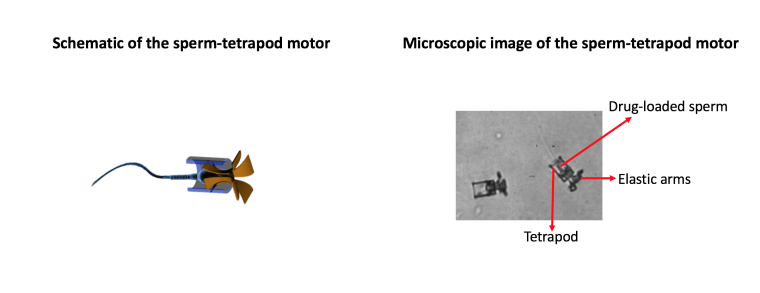
Three days later, only 13 percent of tumor cells were still alive--a level of effectiveness far superior to that seen when doxorubicin was delivered without spermbots.
The scientists foresee a day in which patients with gynecological cancers might lie inside a magnetic chamber where an electromagnetic field would direct the sperm cells to their target. “It would be somewhat similar to lying inside an MRI machine,” says Haifeng Xu, lead author of a paper describing the research.
