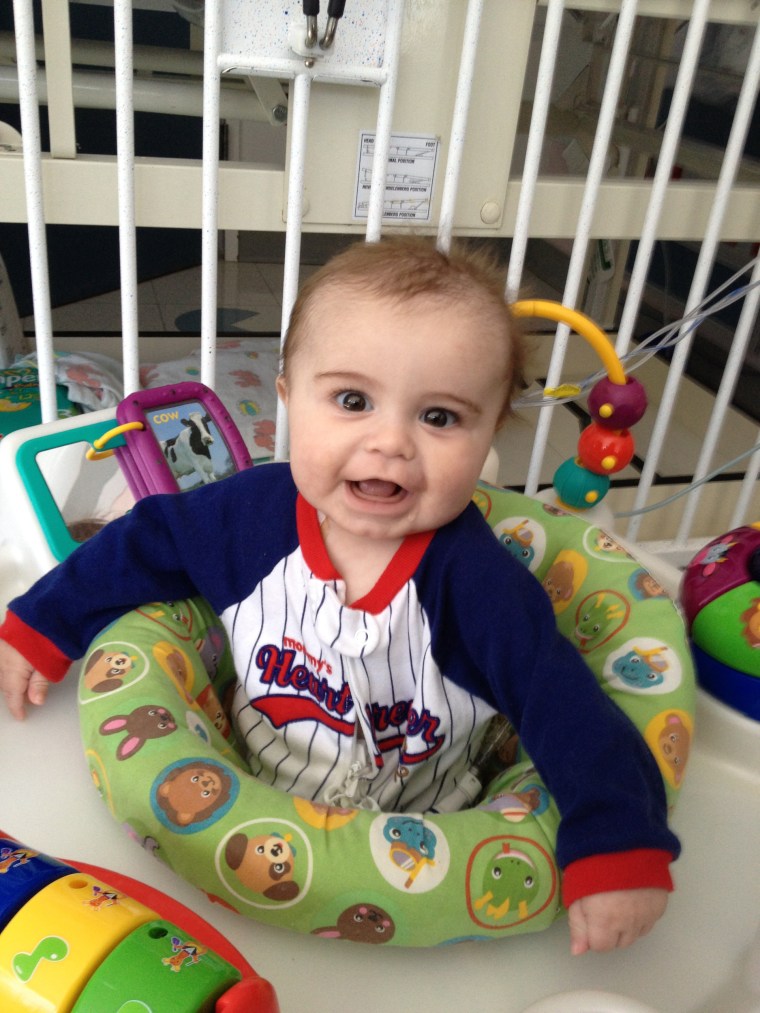
From birth, Northern California newborn Ryland Joseph always seemed happy with a constant smile and twinkle in his brown eyes. But just four months after he was born, the child was diagnosed with Wiskott-Aldrich Syndrome, a rare genetic disorder.
His parents, Rodd and Kellie Joseph, knew their son's only chance for survival was a bone marrow transplant. They chose the highly regarded Benioff Children’s Hospital at the University of California San Francisco Medical Center for the procedure.
But after a successful operation, the boy's health took a serious turn just days later. He died on May 16, 2013. The Josephs said they were shocked to learn Ryland didn't die as a result of the transplant or even his genetic disorder — he died from the Legionnaires' disease that he contracted in his own hospital room.
"I was angry like I've never been angry in my life. This was my only son," Rodd Joseph told NBC News. "I mean, had they tested for it, my son might still be here."
Since the Legionnaires bacteria was first identified after scores of men fell ill at Philadelphia’s American Legion Convention in 1976, thousands are still sickened every year in the U.S., even though some experts say it's almost entirely preventable.
At risk in particular are hospitals, with unsuspecting patients — even babies — vulnerable to a killer in the water.
Most people get Legionnaires by breathing in mist from water that contains the bacteria. It can cause severe pneumonia.
At Benioff Children’s Hospital, Ryland, who had a weakened immune system, was in a special unit away from other people and sources of infection.
The hospital had a policy in place prohibiting "tub baths or showers" in the rooms which would have prevented the spread of Legionnaires through the inhalation of microscopic water droplets.
But hospital cleaning personnel violated that policy by turning on the shower.
The Legionella bacteria thrives in warm water environments like cooling towers and large plumbing systems, but the hospital hadn't tested for it since 2006.
"It was a shock to me," Kellie Joseph said. "And I think that people need to be aware of what it is, and that it’s lurking, and it’s in the hospitals."
Related: Legionnaire's Outbreaks Par for the Course, CDC Says
The Josephs sued the UCSF Medical Center for the wrongful death of their son. The case was later settled out of court.
In court documents, the hospital admits that Ryland contracted Legionnaires' Disease in their facility.
The hospital states it had been using Legionella mitigation practices consistent with industry standards, such as heating water to a certain temperature as it comes into the building from the city, and that it implemented new policies after Ryland’s death.
"UCSF continues to use those practices, and has added a number of other safety measures, such as point of use filters in the rooms of at risk patients, adding tankless water heaters where possible, and adding disinfectant injection points to the water system," the statement said.
In addition to hospitals, Legionella bacteria has been discovered in hotels, veterans homes, even schools.
Twelve people died after Legionnaires was discovered at a veteran’s home in Quincy, Illinois in August, whila a dozen more died this summer in the Bronx, New York, after an outbreak at a hotel.
Special Pathogens Laboratory, based in Pittsburgh, has been testing thousands of water samples from buildings in New York City.
The city mandated testing after the outbreak. At least 30 percent of the samples have tested positive for Legionella bacteria, which doesn’t surprise Dr. Janet Stout, one of the world’s leading Legionella researchers and co-founder of Special Pathogens.
She estimates that each year, roughly 30,000 people contract Legionnaires' disease in the United States and 6,000 die from it. Those figures are higher than government estimates because Stout says cases are under-reported.
According to the Centers for Disease Control and Prevention, the number of Legionnaires cases tripled in the decade between 2000 and 2009. Stout says that could be due to a number of issues, including better detection and diagnosis as well as environmental factors.
She and her partner, Dr. Victor Yu, began their studies in Legionnaires' disease in 1980.
"If you had told me 30-plus years ago we’d be sitting here talking about all these outbreaks and why there isn’t more being done for prevention, I would have been amazed," Stout said.
Stout says hospital patients with weakened immune systems are particularly vulnerable.
"There are people in public health that are afraid to tell people that this bacteria survives water treatments in our water systems," Stout said. "The thing we hear about is we don’t want to start panic. We don’t want to alarm people unnecessarily. So what happens is inaction. The hospitals don’t test their water because the Center for Disease Control and Prevention says wait until there are cases before you go looking for the source. And we think that’s backwards."
Since the outbreaks this summer, a growing number of doctors, scientists, university researchers and former government officials are echoing calls for more proactive testing. The World Health Organization also recommends monitoring for Legionella.
While some state and local municipalities require testing for Legionella and engineering organizations have recently issued new industry standards, the federal government has no such protocols.
Stout says it’s like driving blind, and a case like Ryland Joseph should have never happened.
"Look for Legionella in the water now. Assess the risk. Control the risk," she said. "Because we have tools to do that. And then people don’t get sick and die."
