A new kind of cancer study supports the idea that traditional treatment can be turned on its head, with patients given targeted therapy based not on where their tumors started but on their own genetic mutations.
Researchers used a targeted melanoma drug to treat patients with a range of cancers, from lung cancer to brain cancer, who weren’t being helped by traditional chemotherapy any more. Even though they had many different types of tumors, they all had one thing in common — a genetic mutation called BRAFV600.
It’s a mutation familiar to doctors who treat melanoma, the deadliest form of skin cancer. It’s seen in about half of melanoma cases. A pill called vemurafenib, sold under the brand name Zelboraf, specifically targets the mutation. It helps about half of patients with melanoma who have the mutation.
The same mutation is sometimes seen in colon cancer, lung cancer, thyroid cancer, brain tumors and some blood cancers.
Dr. David Hyman of Memorial Sloan-Kettering Cancer Center and colleagues gathered up what they called a “basket” of 122 patients who had 15 different cancer types and also happened to have a BRAFV600 mutation. They gave them Zelboraf to see what would happen.
“We picked the diseases we thought are the most likely to have this mutation,” Hyman told NBC News.
What they got was a mixed bag. Their findings, published in the New England Journal of Medicine, show that it’s too early to give up completely on the idea of treating cancers based on where they start — the lung, the colon or the breast. But for the patients who were helped, the results were sometimes dramatic.
MaryAnn Anselmo is one example. The 59-year-old jazz singer was diagnosed with a hard-to-treat brain tumor called glioblastoma in 2013, and a few months later, after surgery and radiation therapy, it was clear the tumor was growing again.
"We see no tumor on the scan.”
“We were running out of options, and that’s when I was approached by Dr. David Hyman,” Anselmo, who lives in Morganville, New Jersey, told NBC News.
“He was my lifesaver. He looked at the scans and said, ‘I think I can help you.'”
For Anselmo, the targeted pills worked better than anyone had hoped.
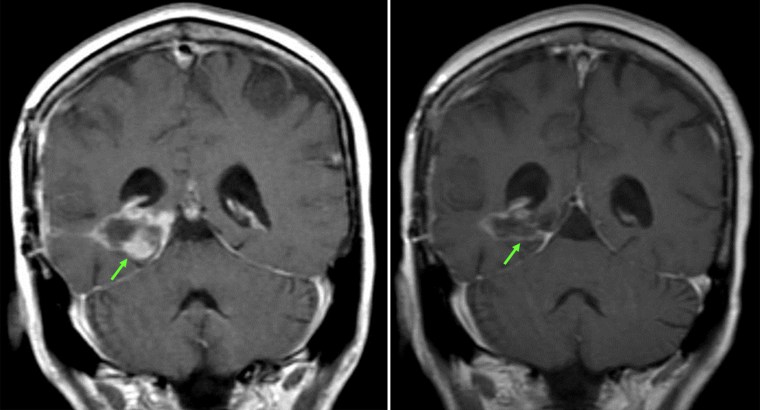
“She started receiving treatment with Zelboraf and, almost immediately, she started to improve clinically,” Hyman said. “Her ability to think and play piano improved. Her tumor shrank, now (on) her most recent CT scan, she’s had a complete response. We see no tumor on the scan.”
Anselmo got her last brain scan earlier this month. “It was just wonderful to hear it was the size of a pea. It was Iike I was given a second chance,” she said.
Some lung cancer patients also got lucky. Hyman’s team tested Zelboraf on 19 stage 4 lung cancer patients with the mutation.
“These are patients who failed multiple chemotherapies,” Hyman said. But the tumors shrank in 14 out of the 19 patients who took the pill, about eight of the patients had a lasting response and five are still taking the pill.
Lung cancer is usually a death sentence, especially stage 4 cancer, so anything that helps is good news. But only 2 percent of lung cancer patients have this BRAF mutation in their tumors — and the study shows not all of them can be helped by the pill.
The best results were seen in a condition that not all doctors agree is truly cancer. It’s called Erdheim-Chester disease, a very rare disorder in which the immune system produces excess quantities of cells called histiocytes. These cells damage the brain, kidneys and other organs. Half of Erdheim-Chester patients have the BRAF mutation.
“It was a true home run in this study,” Hyman said. “Not only did 40 percent meet strict criteria for response, but nearly all of them had improvement in their symptoms and no one progressed while receiving the medicine.”
He said some patients have lived three years. “They are in almost complete remission living their lives on this medicine,” he said.
Colon cancer was a failure, however. Colorectal cancer patients with the BRAF mutation were not helped by the pill, probably because other mutations help drive colon cancer, Hyman’s team reported.
“We want to promote a sense of hope and enthusiasm but also a sense of realism,” Hyman said.
There are some choices for patients, though. Targeted therapies are available for breast and stomach cancers fueled by a mutation in a gene called human epidermal growth factor receptor 2; lung cancer driven by a different EGFR mutation and a type of cancer called gastrointestinal stromal tumor that’s driven by a mutation in a gene called KIT.
“We want to promote a sense of hope and enthusiasm but also a sense of realism."
The goal is to see if these targeted therapies will help patients with other tumors that happen to have the same mutations.
“Patients are being tested already for these mutations, and for some mutations we already have targeted therapies, many of which are already approved for a specific disease. Patients and doctors have to make decisions about how to use these drugs to treat other cancers for which they are not approved,” Hyman said.
But Anselmo pointed out that it’s not standard in many places to test patients’ tumors for their mutations. “Most people don’t know you can have your tumor tested for mutations. It was my husband who pursued that,” she said.
What Hyman hopes is that his new type of “basket” study will help doctors figure out who can be helped by targeted treatments that might not have been immediately obvious.
“We don’t give up just because it’s a rare disease,” he said.
