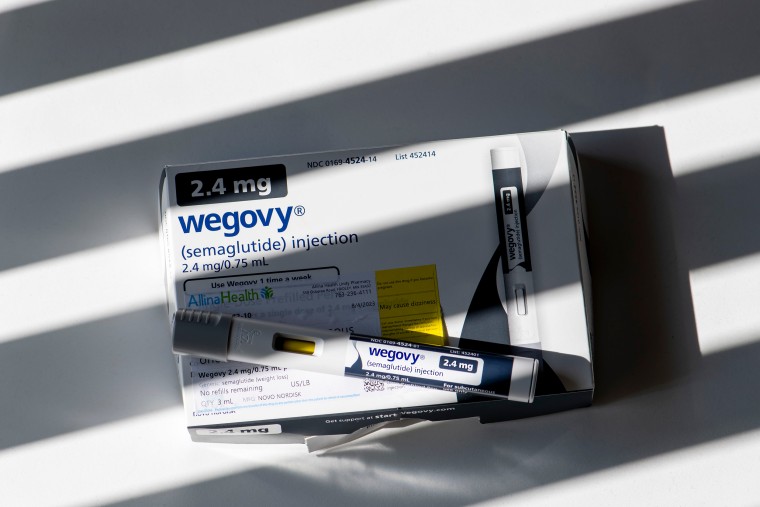
Medicare’s recent move to cover the weight-loss drug Wegovy for some recipients with heart disease risk could drive up the cost of monthly premiums for many of the 65 million adults enrolled in the federal health insurance program, experts warn.
How much of a price jump isn’t yet known. The premium increase would depend on how many millions qualify for the popular medication, which is priced at around $1,300 a month.
It’s possible premiums could go up as soon as 2025, although 2026 or beyond is more likely, according to at least one health policy expert.
“I worry greatly, both in terms of higher premiums and also Medicare funds over the next decade,” said Lawrence Gostin, director of the O’Neill Institute for National and Global Health Law at Georgetown University. “The drug needs to be taken lifelong to be effective, so we’re looking at potentially enormous lifelong costs.”
The drug will be covered under Medicare Part D, which pays for prescription drugs people take at home, according to the Centers for Medicare and Medicaid Services. Last year, more than 50 million of Medicare’s enrollees used Part D plans, according to KFF, a nonpartisan group that studies health policy issues.
This year, people on Medicare Part D pay an average monthly premium of $55.50, according to the CMS. After they meet a so-called coverage gap, patients are on the hook for 25% copays until they spend a certain amount out of pocket, which varies by plan. Part D plans are provided by private insurance companies that have contracts with the U.S. government.
A handful of Part D providers, including CVS Health and Kaiser Permanente, have already said they would start covering Wegovy for patients with heart disease risk. Every major insurance company has been asked for comment.
Under the CMS’ guidelines, Wegovy can be prescribed only to people with heart disease who are either overweight or obese. Medicare won’t pay for Wegovy if it’s being used only for weight loss.
It’s not yet clear how many on Medicare meet those criteria. Juliette Cubanski, deputy director of the program on Medicare policy at KFF, estimated that it is most likely “several million people.”
“If costs go up, then the contribution from the federal government goes up, and generally speaking, beneficiary premiums also go up,” she said.
It’s unlikely that a rise in monthly premiums linked to Wegovy will happen within the next year, said Jeffrey Davis, the health policy director at McDermott and Consulting, a group that provides data analytics and policy advice to the health care industry.
That’s because, he said, private insurance companies that provide Part D coverage have already begun locking in payment rates with Medicare for the 2025 enrollment year.
On the other hand, insurers could still jack up premiums next year if early projections of Wegovy’s costs come in higher than expected, he said.
An analysis published by KFF last month found that gross Medicare spending on the diabetes drug Ozempic, which shares the same active ingredient as Wegovy, increased from $2.6 billion in 2021 to $4.6 billion in 2022, making it the sixth top-selling drug in Medicare Part D that year. Medicare began covering Ozempic in 2018.
However, Davis added, any kind of premium increase caused by Wegovy is much more likely to happen as early as the 2026 enrollment year.
“This drug is expensive,” Davis said. “If millions of people are covered, it could increase premiums going forward.”
Cubanski said even a few dollars in higher premiums can be a big deal for people on Medicare who often are retired and have limited incomes.
Barriers to coverage
It’s important to note that Medicare is allowing insurers that provide Part D coverage to establish rules before they cover Wegovy, a practice that might restrict access in the near term and could keep premiums low, said Gretchen Jacobson, vice president of the Medicare program at the Commonwealth Fund.
Those rules include step therapy, which requires patients to try lower-cost medications before they are allowed to try medications that cost more, Gretchen said.
Some commercial insurers, for example, might start patients off with an older weight-loss medication before they’re allowed to get prescribed a GLP-1 drug.
Insurers can also require Medicare Part D patients to get prior authorization from their insurance companies before they can get the medication.
Dr. Amit Khera, a fellow at the American Heart Association, said that prior authorization is typical for other expensive heart medications and that it’s often a burdensome process for both providers and patients who have to regularly submit medical records and tests showing they meet the requirements for drugs.
“I think the intent is sort of to ensure the right patient gets the right medicine, but practically, it ends up just being an incredibly cumbersome process that, in some ways, can restrict access,” Khera said.
Limiting costs
While insurance companies get a bad reputation for limiting access to patients, Novo Nordisk may also need to share blame for the high cost, Gostin said.
He isn’t alone in that view: Sen. Bernie Sanders, I-Vt., the chair of the Health, Education, Labor and Pensions Committee, last month called on the drugmaker to lower the cost of the drug.
He cited a study by Yale researchers that found that Ozempic and Wegovy could cost less than $5 a month to make, even though Novo Nordisk charges $1,000 a month in the U.S. for semaglutide, the active ingredient in Wegovy.
“I think Bernie Sanders is right to call on them to do that, particularly when it’s selling to Medicare enrollees,” Gostin said.
Even if Novo Nordisk doesn’t lower the prices, semaglutide could be up for Medicare drug pricing negotiations under the Inflation Reduction Act as early as next year, Cubanski said.
The negotiated prices wouldn’t go into effect until 2027.
Davis also said it’s possible insurers providing Part D coverage could negotiate better rebates — discounts drug companies give insurers in exchange for coverage — that could lower the costs for a period of time.