As a New Jersey hospital faced a surge of Covid-19 cases in the spring, another deadly foe was quietly spreading among its patients: a drug-resistant bacterial infection.
The superbug outbreak, detailed in a report published Tuesday by the Centers for Disease Control and Prevention, shows how the coronavirus can overwhelm a hospital, straining care and leaving patients vulnerable to other unwanted outcomes.
Full coverage of the coronavirus outbreak
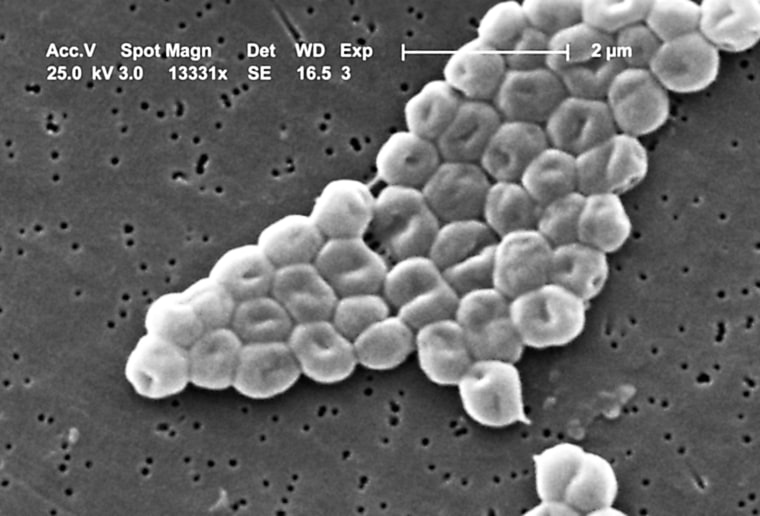
Carbapenem-resistant Acinetobacter baumanii, or CRAB, is a drug-resistant bacterium known to spread in hospitals, particularly in intensive care units. It can cause pneumonia as well as wound, blood and urinary tract infections, according to the CDC. Carbapenem, a powerful antibiotic, is ineffective at treating the infection.
Not all patients get sick — in some cases, the bacteria can "colonize" the body, but not cause an infection. These patients can still spread the bacteria to others.
The outbreak was first detected in the unnamed New Jersey hospital on May 28, according to the CDC report. Further investigation by the hospital and the state health department identified a total of 34 patients who had caught the superbug from February to July. Typically, the hospital sees up to two cases a month.
The majority of the cases — 82 percent — occurred in March through June, when the hospital was facing a surge of Covid-19 patients, and with it, severe shortages in necessary staff, supplies and equipment.
The bacteria pose a threat to hospitalized patients because they can survive on surfaces for a long time, according to the CDC. Contaminated surfaces must be rigorously cleaned and disinfected to prevent outbreaks.
Download the NBC News app for full coverage of the coronavirus outbreak
Such infection control measures, however, took a hit during the hospital's Covid-19 surge. Personal protection equipment was reused, for example. Fewer screening tests for the bacteria were given to patients, because of staff shortages and higher-need patients.
The report also noted that before the pandemic, key parts of a ventilator were changed every 14 days. To conserve equipment during the surge, however, the hospital switched to replacing these parts only when they were visibly soiled or malfunctioning.
Twenty-five of the 34 patients either infected or colonized with the bacteria were on ventilators at the time.
Twenty of the 34 patients did become infected, including 11 patients with Covid-19. Fourteen developed a form of pneumonia linked to the bacterial infection, four of whom also had bacteremia, a blood infection. A total of 10 patients died, and one remains hospitalized, according to the report.
It wasn't until late May that the hospital was able to resume normal operations — and with that, CRAB cases fell.
Follow NBC HEALTH on Twitter & Facebook.