You should not wake up and dread taking your first step of the day. If you do, there’s a pretty good chance you have plantar fasciitis, an uncomfortable foot condition that anyone can get for a laundry list of reasons: wearing the wrong shoes, overextending yourself while working out, losing or gaining weight and going through menopause are just a few.
“Feeling pain when you take your first step in the morning is a hallmark sign of plantar fasciitis,” says Dr. Priya Parthasarathy, a podiatrist at the Foot & Ankle Specialists of the Mid-Atlantic. “Patients tend to ignore it because it usually goes away once you start moving, but it can advance to pain after activity, during activity or all the time.”
If you address symptoms as soon as you feel them, plantar fasciitis is relatively easy to deal with — and conservative treatments like stretching, icing and massaging work 90% of the time, says Dr. Jacob Wynes, a podiatric surgeon and an associate professor of foot and ankle surgery for the University of Maryland Medical System. Keep scrolling to learn more about what to do if you have plantar fasciitis and tools that help alleviate pain. The doctors also explain when the condition is most common. Spoiler alert: It’s right now.
Want more from NBC Select? Sign up for our newsletter, The Selection, and shop smarter.
What is plantar fasciitis?
Plantar fasciitis is a condition that causes pain in the plantar fascia, a ligament that runs along the bottom of your foot to support it, says Wynes. The pain results from micro-tears that develop along the ligament, leading to inflammation. At first, you’ll likely feel occasional pain around the heel, or pain when you take your first step after resting for a while, like first thing in the morning. But if plantar fasciitis is left untreated, it can advance to around-the-clock pain anywhere along the ligament and affect the alignment of your knees, hips and ankles, says Parthasarathy.
How to treat plantar fasciitis, according to podiatrists
If you suspect you have plantar fasciitis, first consult your podiatrist to rule out other issues, like nerve damage, stress fractures, bursas and bone spurs. Once you have a positive diagnosis, you can start conservative treatments — Wynes says they almost always work if you do them consistently. Your podiatrist will evaluate how you respond to that regimen after a few weeks — depending on progress, they might suggest advanced treatments.
“I always tell my patients that you need to do three things to address plantar fasciitis: support the foot, stretch the plantar fascia and reduce inflammation,” says Parthasarathy. I detail the most common conservative treatments for plantar fasciitis below and recommend the tools you’ll need for them, per podiatrists’ guidance.
Stretch with resistance bands
Stretching is nonnegotiable when you’re treating plantar fasciitis. Dr. Bobby Pourziaee, a podiatrist at Rodeo Drive Podiatry based in Beverly Hills, California, recommends getting a light resistance band (like those in the pack below), putting it over the ball of your foot with your knee straight, holding it with both hands and gently putting your foot toward you. Stretch one foot for 30 seconds, then the other, then repeat. “Even if one of your feet isn’t symptomatic, you should do the stretch on both sides so they’re even,” says Pourziaee. Beyond targeting the back of the foot, this stretch releases the calf muscles and the Achilles tendon, which are all connected, says Wynes.
It’s best to stretch first thing in the morning before your feet even touch the ground, so consider keeping the resistance bands on your nightstand and stretching in bed. Pourziaee also suggests doing a second round of stretching at the end of the day. You can take a Nonsteroidal Anti-Inflammatory Drug (NSAID) to help with pain and inflammation, too, like Advil, Motrin, Aleve and aspirin.
You get three non-latex resistance bands in this set, and they’re color-coded to indicate resistance level: the light band is yellow, the medium band is red and the heavy band is green. They’re each 5 feet long, giving you plenty of room to wrap around your foot, and 4 inches wide, helping them stay in place while you’re stretching. The bands take up practically no room in your bag, so you can easily travel with them or bring them to the gym, as well as keep a set at home to stretch at least twice a day.
Ice the bottoms of your feet
After stretching your feet, ice them — it’s another nonnegotiable. There’s no right or wrong way, but to really target the plantar fascia, all the experts recommend buying a large disposable water bottle, freezing it and rolling your foot back and forth on top of it for three or four minutes. There’s also reusable ice packs (which I included examples of below) specifically designed to hug the bottoms of your feet, and others that have a ball-like shape to mimic the type of massage you get from the water bottle. Parthasarathy recommends icing twice a day.
This reusable, gel-filled ice pack covers the heel, ankle and bottom of your foot, and it’s compatible with the right and left sides. You secure it in place with a stretchy adjustable strap that can also add compression depending on how tightly you wrap it. Comfpack recommends freezing the ice pack for 4 hours before using it, or you can put it in the microwave for 30 seconds to use it as a heating pad. It typically stays cold for over 30 minutes once you take it out of the freezer, and it remains flexible even when frozen, according to the brand.
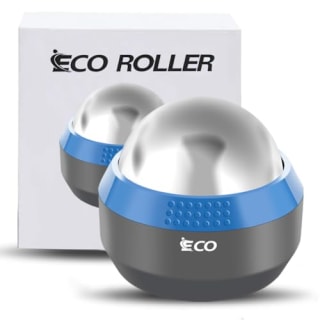
If you want to ice and massage your plantar fascia at the same time, but don’t have room in your freezer for a large disposable water bottle, try this stainless steel roller ball. It’s sized to fit in the palm of your hand, letting you hold the base and roll it along the bottom of your foot or put it on the ground and roll your foot on top of it. The ball is filled with a cooling gel that’s activated when you put it in the freezer for two hours, and it stays cold for about 6 hours, according to the brand. You can also use it for heat therapy by screwing the steel ball off its base, placing it in hot water for up to 10 minutes, re-attaching it to the base and massaging where needed.
Massage the bottoms of your feet
“Massaging stimulates blood flow, which is really good for the damaged plantar fascia,” says Pourziaee. It accelerates the body’s natural healing process by bringing oxygen and other nutrients to the ligament’s micro-tears, which can help repair them and decrease inflammation. Rolling a frozen water bottle underneath your foot accomplishes icing and massaging at once, but you can also buy little foot massaging gadgets, which Pourziaee says can’t hurt to try.
Chrip’s compact, portable massage roller is designed to fit under your foot, letting you roll it back and forth along the plantar fascia to loosen up the ligament. The tool’s nodes mimic a thumb massage, helping it target sore spots and pressure points, while its texture adds grip. It’s made from firm foam with a rubber exterior.
Sleep with a night splint
Your feet naturally point down while you’re sleeping, which has a shortening and tightening effect on the plantar fascia and Achilles tendon, says Pourziaee. This position exacerbates plantar fasciitis-related pain, especially when you take your first step in the morning: You’re suddenly putting all of your body weight on and abruptly stretching an inflamed ligament that got extra tight overnight, which is technically called post-static dyskinesia, says Wynes.
Night splints are a solution to this problem. “It’s basically a stretcher for your foot,” says Pourziaee. “The splint straps onto your foot and connects to your leg, keeping your foot at 90 degrees while you’re sleeping and stretching it overnight.” Before trying a night splint, talk to your podiatrist to make sure it’s the right choice for you since there’s a few cons: “If it’s too tight, patients say it hurts or they get numbness, so you have to play around with it,” says Pourziaee.
This is a standard night splint for plantar fasciitis. It keeps your foot at a 90-degree angle once you secure it in place, and you can customize the stretch intensity level using the adjustable straps. The splint also comes with a removable wedge that adds additional stretch if you want it. To keep you comfortable overnight, the boot has padded foam and a soft interior lining, as well as a slip-resistant sole. It’s available in small, medium and large sizes — be sure to use the brand’s size chart to find the best fit for you.
Add shoe inserts to footwear
Shoe inserts replace the standard insoles footwear comes with, and they’re specifically designed to offer more support and cushioning while improving fit. There’s lots of generic inserts available over the counter, or your podiatrist can make you a custom set (called orthotics) that targets the exact issues you’re dealing with.
All the podiatrists I spoke to say custom orthotics are more beneficial than over-the-counter inserts, but they can cost hundreds of dollars and aren’t always covered by insurance. If you’re interested in orthotics but want to spare yourself the cost, high quality inserts are still helpful. Wynes recommends looking for a pair that aligns with your arch type (neutral, flat or high) and has a three-quarter length shell. (The shell of a shoe insert is the rigid interior part that does the majority of the work to support your feet.) “A three-quarter length insert is more efficacious than a full-length insert because it suspends the arch and supports the plantar fascia better,” says Wynes, noting that the insert’s cover (the exterior part that actually touches your foot) can be longer.
Pourziaee says Superfeet makes some of the best over-the-counter shoe inserts. They come in specialized options for activities like running and hiking, as well as all-purpose models to wear daily. The all-purpose insoles have three layers: a 3/4-length stabilizer cap that’s the main supportive and structural element; a firm, thick piece of shock-absorbing foam; and a moisture-wicking, odor-reducing cover. They’re also designed with a deep, sculpted heel cup. You can trim the inserts to fit your shoes, so they’re compatible with most footwear, according to the brand. You can buy the all-purpose inserts for neutral, high and flat arches. You’ll need to swap them out for a new pair about every 12 months.
Reconsider your footwear
If you actively have, or have a history of, plantar fasciitis, stay away from unsupportive shoes, especially those like flats and very high heels, says Pourziaee. Look for footwear that has the following features, and make sure you’re getting a new pair of shoes every 300 to 500 miles, says Parthasarathy.
- The right type of arch support for your feet. If you don’t know your arch type, use our guide or talk to your podiatrist. In general, you can tell whether a shoe has arch support by trying to fold it in half: The more it folds, the less arch support it has, says Parthasarathy.
- A deep heel cup, which supports the heel bone (the calcaneus) and prevents it from excessively moving around.
- A firm heel counter, which is the U-shaped piece inside a shoe that hugs your heel to keep it stable and prevent slippage. “The heel counter should be rigid enough that it doesn’t fold and bend when you squeeze it,” says Wynes.
- A thick sole to absorb shock
- Flexibility balanced with structure. “You want to make sure it bends at the ball of the foot, but you can’t squish or fold it in other places,” says Pourziaee. Look for rigid shoes that can’t twist much, if at all — they help your foot go through all phases of a gait cycle (flat foot, heel off, toe off) and take strain off the plantar fascia, says Wynes.
- A removable insole, letting you add shoe inserts or orthotics
Here are two of experts favorite sneakers for plantar fasciitis. They each have all of the features listed above.
Pourziaee and Parthasarathy both recommend Hoka’s Bondi sneakers (available in men’s and women’s sizes) if you have plantar fasciitis. “They have a slight rocker bottom outsole that helps take away from the stress on the plantar fascia and stretches it out a bit,” says Pourziaee. He also highlights their extra cushioning, which gives excellent shock absorption — just be aware that the thick layer of foam lifts you off the ground by a few inches, so if you struggle with stability or balance, Parthasarathy suggests opting for the slightly less cushioned Hoka Cliftons instead. The Bondis are designed with a molded collar to hold your feet in place, grippy rubber outsoles, reflective details and breathable mesh fabric.
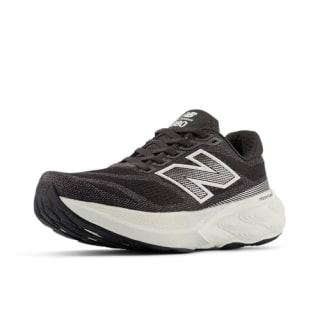
These sneakers (available in men’s and women’s sizes) are another one of Parthasarathy’s favorite options for those with plantar fasciitis. “The 880s work for a lot of different foot types, and New Balance’s sneakers come in excellent widths,” she says. The sneakers have a moderate amount of soft cushioning, a stable base, breathable mesh fabric and a gentle rocker-shaped rubber outsole for smooth heel-to-toe transitions.
Don’t go barefoot at home
Most people’s homes are covered in hard flooring that has no shock absorption, like engineered hardwood and tile. Constantly walking barefoot on this surface adds stress to and strains the feet, aggravating conditions like plantar fasciitis, says Parthasarathy. “Home shoe gear is just as important as outdoor shoe gear when you’re battling plantar fasciitis,” she says. “I recommend wearing slippers or sandals with arch support, not flats.” Below are two of her top picks.
Once I slipped my feet into these slides (available in unisex sizes), my days of walking around barefoot at home were over. They give my feet a cushy, comfortable place to rest and recover, especially after they’ve been cooped up in running sneakers, boots or loafers for hours. The lightweight slides are made from an impact-absorbing foam that has just enough structure that I never feel like I’m sinking into it. They’re also designed with a rounded, cupped heel for added stability. I find the slides easy to keep on my feet without gripping my toes, and the two bands that rest across the tops of my feet lay flat, preventing them from digging into my skin or leaving marks.
Vionic’s Relax II slippers have a footbed with built-in arch support, a deep stabilizing heel cup and shock-absorbing cushioning. The forefoot of the shoe (the area near the ball of the foot) is flexible while the rest of it is rigid, and the outsole is durable to withstand indoor and outdoor use. You can also customize these slippers’ fit with the adjustable hook-and-loop closure on the faux fur shearling cross strap.
Frequently asked questions
Anything that irritates or damages your plantar fascia can lead to plantar fasciitis, and more times than not, it’s a use or overuse injury, says Wynes. That said, it can also be triggered by certain body changes or trauma to the foot. Some of the most common causes are:
- Wearing worn-down, unsupportive shoes, or shoes that aren’t right for your foot type. Parthasarathy sees an influx of patients with plantar fasciitis during the transition from summer to fall for exactly this reason: “I always call it plantar fasciitis season because people wear poor shoes all summer, like flip flops, and it catches up to them,” she says.
- Wearing the wrong shoes for a specific activity. Parthasarathy sees an uptick in patients with plantar fasciitis in January and February because they started new exercise routines at the beginning of the year, but they weren’t wearing the right shoes or recovering properly.
- Standing for long periods of time. Pourziaee says many of his patients that have plantar fasciitis are retail workers and those who work in the food service industry.
- Doing certain physical activities, including those that involve repetitive pounding, like running, or repetitive jumping, like HIIT workouts.
- Having flat feet, which typically causes you to overpronate, meaning the foot rolls inward, putting a lot of strain on the plantar fascia, says Pourziaee
- Having high arches, which prevents the plantar fascia from being able to adequately stretch, causing it to tighten up, says Wynes
- Weight loss or gain
- Hormonal changes, like during perimenopause, menopause and pregnancy
Plantar fasciitis doesn’t heal overnight: You’re on your feet every day and can’t fully rest them like you can with other areas of your body if they’re injured, says Parthasarathy. Mild cases of plantar fasciitis typically take a few weeks to heal while following a consistent icing and stretching regime, says Pourziaee. If you’re still experiencing pain when you see your podiatrist for a follow up appointment, and icing and stretching hasn’t made noticeable improvements, they may recommend advanced treatments like physical therapy or cortisone shots after getting imaging done. Surgery for plantar fasciitis is very rare, experts say.
Plantar fasciitis can go away after treating it, but if you don’t make the necessary lifestyle changes to support your feet and prioritize recovery, you may be susceptible to getting it again, says Parthasarathy.
“If you have plantar fasciitis, I recommend cutting down your activity by at least 50%, including how many steps you take a day,” says Parthasarathy. Not reducing your activity leads to further inflammation, which erases progress you make with treatments like icing and stretching and takes you longer to recover. That doesn’t mean you can’t exercise at all — you just have to be intentional about how you’re moving your body.
Those with plantar fasciitis should limit high-impact activities that involve repetitive pounding, like running, and jumping, like HIIT workouts, which can increase inflammation in the plantar fascia, says Pourziaee. Also, don’t hike or walk on rocky, uneven terrain. Instead, opt for low-impact cardio on the elliptical machine, which has a stretching effect on the legs and feet, bike (indoors or outdoors) or rowing machine, and consider swimming or water aerobics. Experts also suggest doing more stretching, lengthening and strengthening activities like yoga, Pilates and upper body weight lifting.
After a case of plantar fasciitis heals, Pourziaee recommends continuing a simple icing and stretching regime as a preventative measure, especially if you’re very active and/or on your feet a lot, as well as after strenuous exercise or a challenging training day. Other than that, the best way to prevent plantar fasciitis is to make sure you’re always wearing supportive shoes that are compatible with your foot type, and adding inserts to footwear as needed.
Meet our experts
At NBC Select, we work with experts who have specialized knowledge and authority based on relevant training and/or experience. We also ensure that all expert advice and recommendations are made independently and with no undisclosed financial conflicts of interest.
- Dr. Jacob Wynes is a podiatric surgeon and an associate professor of foot and ankle surgery for the University of Maryland Medical System.
- Dr. Priya Parthasarathy is a podiatrist at the Foot & Ankle Specialists of the Mid-Atlantic.
- Dr. Bobby Pourziaee is a podiatrist at Rodeo Drive Podiatry based in Beverly Hills, California.
Why trust NBC Select?
I’m a reporter at NBC Select who has covered health and wellness for over five years. I’ve written numerous articles about footwear and foot health, including topics like blisters, arch types, running sneakers, walking sneakers and training shoes. To write this article, I interviewed three podiatrists, who shared information about plantar fasciitis treatments. Using their guidance, I curated a list of products that can aid healing.
Catch up on NBC Select’s in-depth coverage of tech and tools, wellness and more, and follow us on Facebook, Instagram, Twitter and TikTok to stay up to date.